
Life and Death in a Glass of Water: Cholera
2025-09-19
Introduction
How many times do you drink a glass of water per day? Perhaps four to five glasses a day? Maybe if you are a hydration enthusiast, you drink much more than that. Nevertheless, living in Canada, we tend to worry about the amount of water we drink, not the consequences that we will face when we drink water. Unfortunately, for marginalized individuals in low socio-economic countries such as Myanmar, Sudan, South Sudan, and the Democratic Republic of Congo, every sip of water can be life and death due to cholera.[1] It is estimated that in the 69 endemic countries studied, 2.9 million cases of cholera are detected with 95,000 deaths every year.[2] In the same study, it was found that a large portion of these endemic countries is in Sub-Saharan Africa, with the World Health Organization (WHO) reporting a 125% increase in cases in Africa in 2023, while countries in the Middle East and Asia showed a 32% decrease in prevalence.[2,3]
Cholera is no joke, and the resurgence of this neglected tropical disease is of great significance for epidemiologists, a field of science that focuses on the study of disease transmission. But what is Cholera, and why is it so deadly? Today, we will take a dive into the microbial environment in water to closely examine the pathogens that cause the disease, the transmission dynamics and conclude with the current treatment and prevention regimes.
Pathogenesis of Cholera
Our first question is, “What is Cholera?” To understand this disease, we must direct our eyes to the microscope to view the tiny troublemaker. Cholera is caused by a gram-negative bacteria called Vibrio cholerae (V. cholerae), which has a distinct curved rod shape, as seen in Figure 1. This bacteria has a single polar flagellum, a long tail-like structure on the bacterium, that gives it the ability to tread through the aquatic environment in which it thrives.[2,4-6]
These bacteria contaminate water and are found, especially in brackish water, estuaries, and coastal areas, as a free-living cell or a thoroughly organized gel-like colony called a biofilm.[4-6] The human consumption of water contaminated with V. cholerae leads to acute gastrointestinal diarrheal disease with symptoms including watery diarrhoea and vomiting.[6,7] While symptoms may be mild for healthy individuals, some patients experience much more severe symptoms that can lead to deadly complications, such as hypovolemic shock, acidosis, and even death if untreated.[4-7]
Now that we have identified the causative agent, we can transition to our next big question: “What is the disease mechanism of Cholera?” V. cholerae enters the body by ingestion of contaminated water or food. While the stomach has a high pH, V. cholerae can bypass these harsh environments. What is interesting about V. cholerae is its unique ability to adapt quickly to environmental changes. Whether it be a change in salt concentrations, pH, osmolarity, or the presence of bile salts in the human host, it has complex machinery called virulence factors to adapt and reproduce in the environment.[6] Once the bacteria pass the stomach, they enter the small intestine. Their flagellum motor and the mucinous enzyme work together to penetrate the mucus layer and attach to the intestinal epithelial cells. Here, the V. cholerae colonizes and adheres to the intestine to cause havoc in the cell.[5,6]
The bacteria have infiltrated our first line of defence into the small intestine, but now what happens? What is causing the diarrhea and severe dehydration? The primary virulence factor that causes all these symptoms is the deadly cholera toxin (CT). CT is what is called an “A-B type toxin” that is composed of two proteins, A and B.[8] The A component is the pathogenic enzyme component, and the B component is the receptor binding domain.[9] For clarity, we will refer to the A component as the Attacker and the B component as the Binder. The binder is specific to and recognizes a receptor on our intestinal epithelial cells called GM1 ganglioside receptors. The binding engulfs the CT, internalizing the toxin in a process named endocytosis. CT’s attacker can now travel freely inside the cell’s fluid-like cytoplasm.[9] CT looks for a complex cellular signalling receptor named G-protein coupled receptor (GPCR). Normally, GPCR is involved in creating a messenger molecule called cyclic AMP (cAMP). These cAMP concentrations are held at a relatively stable level to appropriately communicate within the cell. However, the attacker in CT will catalyze the ADP-ribosylation of the Gs-α subunit of the adenylate cyclase enzyme, preventing GTP hydrolysis and causing an over-accumulation of cAMP.[4,8] This may sound confusing, but in simple terms, the attacker disrupts the normal level of cAMP by removing the off-switch of the cAMP factory in our cells.
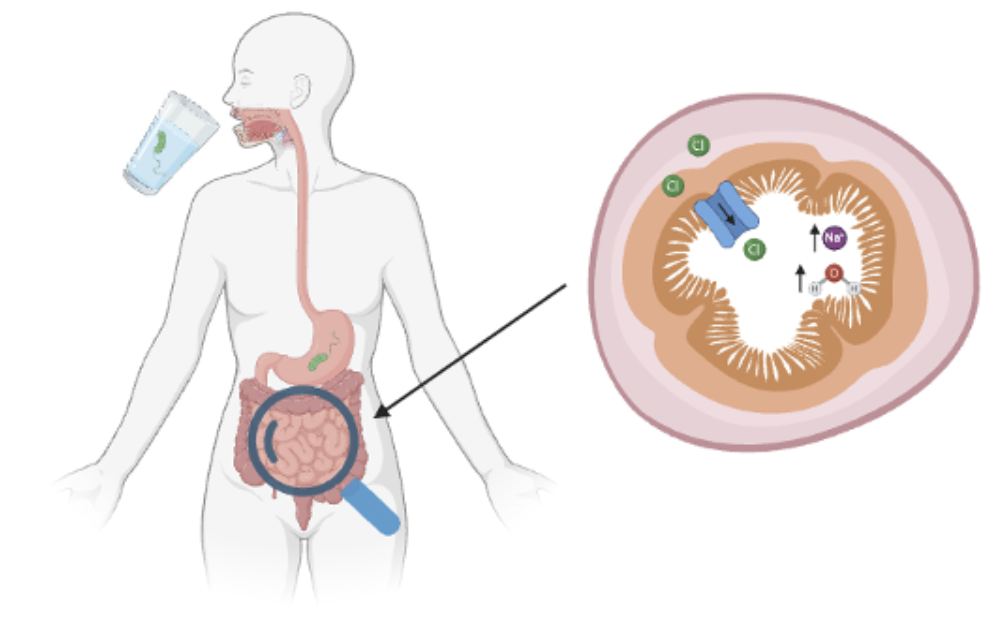
Once there is a flood of cAMP, these molecules communicate to downstream effectors such as protein kinase A (PKA). PKAs are a set of enzymes that put a phosphate group onto a protein they want to switch on, much like an alarm waking you up in the morning. In this case, PKA wakes up the protein, cystic fibrosis transmembrane conductance regulator (CFTR), an ion channel that, when awake, provides a highway for chloride ions to move into the intestine.[4] The high concentration of chloride ions in the intestine now disrupts the absorption of other essential ions, such as sodium. This ion imbalance causes the inside of the intestine to be salty, leading to an osmotic gradient.[8] Now, what happens when we eat something salty? We drink water. Similarly, when the intestine is rich in ions, water molecules travel to that site because of the osmotic gradient. Therefore, due to the excessive water in the small intestines, the once-solid stool becomes watery, causing diarrhea. Moreover, water loss within our intestinal cells causes large systemic dehydration in our bodies, deadly if not treated.[8]
Challenges in Controlling Cholera
As we can see, our body has incredible immune systems that have great tactics to protect us from V. cholerae. Then why are the cases in countries like South Africa increasing? The issue lies in the several public health challenges that are presented in such marginalized countries. The very core of the Cholera epidemic is not the inability of the immune system. Poor sanitation, inadequate healthcare infrastructure, and climate change. [1,3,7,13,14]
Poor sanitation and lack of access to safe, clean water for consumption are key drivers of the upward trend. In many regions, people rely on contaminated water sources due to poor municipal water sanitation. This highly vulnerable population even include children and babies.[13] Furthermore, it was reported that Cholera spreads at unimaginable rates in overcrowded urban slums with poor water management, leading to these individuals relying on sewage-contaminated water for consumption.[7,13] The heartbreaking photo from the Voice of America’s recent news article depicts the reality for African children who obliviously risk their lives daily for an essential human need.[13]

Climate change is another driver of the ever-increasing cases of Cholera in Africa. Extreme weather patterns, including severe floods and droughts.[14] Unpredictable floods exacerbate Cholera due to the rise in water levels that spill over Cholera-contaminated water into clean sources. This phenomenon has been shown to lead to never-ending outbreaks. To make matters worse, droughts reduce water availability for individuals, increasing their probability of resorting to contaminated water for survival.[14]
The Call for Action
Cholera is one of the most urgent epidemiological issues in the 21st century. Despite the availability of vaccines and antibiotics for V. cholerae, the global vaccine supplies are insufficient to supply the growing demand.[1] Vaccine shortages have left millions of individuals vulnerable. The international health community must emphasize improving sanitation, access to safe water, education on basic hygiene principles, and increasing vaccine supply at a cheaper price point. Recently, organizations such as the World Health Organization have committed significant efforts to improve the hygiene and water sanitation infrastructure using the WASH intervention as a long-term solution for controlling cases of cholera.[7] While the intervention has shown some promising results, it is not yet enough.
Life and death are not a matter of yes, no, and maybe. It is a human right to have an adequate supply of safe drinking water. For us, it is important to be aware and raise awareness on this urgent yet neglected matter. So today, as you drink your cup of water, understand and share the word about cholera. It is only together that the children and adults of low-socioeconomic countries can comfortably drink the water as we do.
References
1. Lay K, Salih ZM, Miettaux F. Dirty water and endless wars: why cholera outbreaks are on the rise again [Internet]. Juba: The Guardian; 2025 [updated 2025 Feb 11; cited 2025 Mar 10]. Available from:
2. Ali M, Nelson AR, Lopez AL, Sack DA. Updated Global Burden of Cholera in Endemic Countries. PLoS Negl Trop Dis [Internet]. 2015 Jun [cited 2025 Mar 10];9(6):e0003832. Available from: (DOI: 10.1371/journal.pntd.0003832)
3. World Health Organization. Cholera, 2023. Wkly Epidemiol Rec [Internet]. 2024 Sep [cited 2025 Mar 10];99(36):481-495. Available from:
4. Kumar A, Das B, Kumar N. Vibrio Pathogenicity Island-1: The Master Determinant of Cholera Pathogenesis. Front Cell Infect Microbiol [Internet]. 2020 Oct [cited 2025 Mar 10];10:561296. Available from: (DOI: 10.3389/fcimb.2020.561296)
5. Hsiao A, Zhu J. Pathogenicity and virulence regulation of Vibrio cholerae at the interface of host-gut microbiome interactions. Virulence [Internet]. 2020 Nov [cited 2025 Mar 10];11(1):1582-1599. Available from: (DOI: 10.1080/21505594.2020.1845039)
6. Ramamurthy T, Nandy RK, Mukhopadhyay AK, Dutta S, Mutreja A, Okamoto K, Miyoshi SI, Nair GB, Ghosh A. Virulence Regulation and Innate Host Response in the Pathogenicity of Vibrio cholerae. Front Cell Infect Microbiol [Internet]. 2020 Sep [cited 2025 Mar 10];10:572096. Available from: (DOI: 10.3389/fcimb.2020.572096)
7. World Health Organization. Cholera. World Health Organization [Internet]. 2024 [updated 2024 Dec 5; cited 2025 Mar 10]. Available from:
8. Bharati K, Ganguly NK. Cholera toxin: A paradigm of a multifunctional protein. Indian J Med Res [Internet]. 2011 Feb [cited 2025 Mar 10];133:179-187. Available from:
9. Zhang L, Leroux JC. Current and forthcoming approaches for systemic detoxification. Adv Drug Deliv Rev [Internet]. 2015 [cited 2025 Mar 10];90:1–2. Available from:
10. Bourque DL, Bhuiyan TR, Genereux DP, Rashu R, Ellis CN, Chowdhury F, et al. Analysis of the Human Mucosal Response to Cholera Reveals Sustained Activation of Innate Immune Signaling Pathways. Infect Immun [Internet]. 2017 Nov [cited 2025 Mar 10];86(2):e00594-17. Available from: (DOI: 10.1128/IAI .00594-17.)
11. Bielig H, Rompikuntal PK, Dongre M, Zurek B, Lindmark B, Ramstedt M, et al. NOD-Like Receptor Activation by Outer Membrane Vesicles from Vibrio cholerae Non-O1 Non-O139 Strains Is Modulated by the Quorum-sensing Regulator HapR. Infect Immun [Internet]. 2011 Apr [cited 2025 Mar 10];79(4):1418-1427. Available from: (DOI: 10.1128/IAI.00754-10)
12. Seper A, Hosseinzadeh A, Gorkiwicz G, Lichtenegger S, Roier S, Leitner DR, et al. Vibrio cholerae Evades Neutrophil Extracellular Traps by the Activity of Two Extracellular Nucleases. PLoS Pathog [Internet]. 2013 Sep [cited Mar 10];9(9):e1003614. (DOI: 10.1371/journal.ppat.1003614)
13. Mavhunga C. UN Concerned by Spread of Cholera to 10 African Countries [Internet]. Washington, D.C: Voice of America English News; 2024 Jan 17[updated 2025 Jan 17; cited 2025 Mar 12]. Available from:
14. Ram A, Singh I. Cholera cases explode after extreme rains fuelled by climate change in west and central Africa [Internet]. Canada: Canada Broadcasting Corporation (CBC); 2024 Oct 23[updated 2024 Oct 23; cited 2025 Mar 12]. Available from:
